Current Issue
Surgical Techniques for Treating RT2-Associated Gingival Recession: A Randomized Controlled Clinical Trial
Malek A Abdulmatlob1, Muna S Elburki1,*, Anas R Elharathi1, Manal S Bazina1, Abdalmawla A Ali2, Omar A Huni3
1Department of Periodontics, Faculty of Dentistry, University of Benghazi, Libya
2Department of Orthodontics, Faculty of Dentistry, Sirte University, Libya
3Department of Periodontics, Libyan International Medical University, Benghazi, Libya
*Corresponding author: Dr. Muna S Elburki, BDS, MPhil, PhD, Assistant Professor, Department of Periodontics, Faculty of Dentistry, University of Benghazi, Benghazi, Libya, Tel: 00218924261466, ORCID: 0000-0003-2657-6078, Emails: [email protected]; [email protected]
Received Date: September 15, 2024
Publication Date: October 29, 2024
Citation: Abdulmatlob MA, et al. (2024). Surgical Techniques for Treating RT2-Associated Gingival Recession: A Randomized Controlled Clinical Trial. Medical Research. 3(1):13.
Copyright: Abdulmatlob MA, et al. © (2024).
ABSTRACT Background: Gingival recession type 2 (RT2) is characterized by the gingival recession associated with loss of interproximal attachment. The interproximal attachment loss is less than or equal to the buccal attachment loss. Various surgical strategies, such as connective tissue grafts (CTG) and coronally advanced flaps (CAF), were employed to deal with this situation. However, the best technique remains controversial. The present study aimed to evaluate and compare the efficacy of different surgical techniques for treating RT2 gingival recessions, focusing on root coverage, clinical attachment level (CAL) gain, keratinized tissue width (KTW) increase, and patient-reported outcomes. Methods: Thirty participants with RT2 gingival recession were randomly assigned to 3 groups: Group A (CTG alone), Group B (CAF alone), and Group C (CTG+CAF). The outcome was assessed at baseline and six months post-surgery. Results: The combined technique (Group C) obtained the superior effects with 82.5% root coverage, a CAL gain of 2.8 mm, and a KTW increase of 1.8 mm. Group A and Group B confirmed 75.3% and 68.7% root coverage, CAL gain of 2.4 mm and 2.1 mm, and KTW increases of 1.5 mm and 1.2 mm, respectively. Patient-reported aesthetic satisfaction turned into highest in Group C. Statistical analysis indicated significant differences in results between the groups (p < 0.05). Conclusions: The combination of CTG and CAF offers the best clinical outcomes and patient satisfaction in treating RT2 gingival recessions. These results support the approval of combined surgical strategies as the ideal technique for treating complex gingival recessions.
Keywords: Recession Type 2, Connective Tissue Graft, Coronally Advanced Flap, Clinical Attachment Loss, Keratinized Tissue Width, Patient Satisfaction
INTRODUCTION
The treatment of RT2-related gingival recession remains a complicated and evolving mission in periodontal surgery [1]. Recession Type 2 (RT2) is defined as gingival recession characterized by loss of interproximal attachment. The interproximal attachment loss was less than or equal to the buccal attachment loss (measured from the buccal CEJ to the depth of the buccal pocket) [1]. This poses demanding situations for oral hygiene and influences the quality of life through compromising aesthetics [2]. The Cairo classification categorizes recession based mainly on interdental CAL measurement [1]. RT2 recessions are particularly difficult, lacking attached gingiva between the tooth and exhibiting bone loss, complicating whole root coverage. Gingival recession results from elements like periodontitis, trauma from brushing, orthodontic treatment, thin gingival phenotype and aberrant frenal attachment [3,4]. Exposed roots compromise aesthetics, and cause caries, and hypersensitivity issues. Losing attached gingiva compromises the periodontium's protective barrier, increasing susceptibility to further recession and disease [2]. Class III recession beyond the mucogingival junction with interdental tissue/bone loss. This kind was proved complicated to deal with completely because of inadequate interdental papillae for tissue regeneration [2].
Different surgical modalities target recession, and each has its strengths, limitations, and acceptable scenario. The main options for treating gingival recession are soft tissue grafts, coronally advanced flaps (CAFs), and combinations of both [5]. Connective tissue grafts (CTGs) and xenogeneic matrices increase tissue volume and promote coverage but are associated with palatal donor morbidity and complications [6]. Methods such as CAFs and tunneled CAFs restore tissue coronally, and show promising results but require keratinized tissue and appropriate handling skills [7,8]. In complex Class III cases, the combination of CTGs and CAFs utilizes the advantages of each option - structural support and regeneration and positional advantages - to deliver results such as coverage, increase keratinized tissue width and aesthetic [5,9].
The purpose of this study is to assess the efficacy and long-term effects of different surgical procedures for the management of RT2 gingival recessions. Specifically, the objectives are: 1. To examine the effectiveness of soft tissue grafts like connective tissue grafts (CTGs). 2. To assess the overall performance of coronally advanced flaps (CAFs) and their variations, which include tunneled CAFs, in treating RT2 recessions. 3. To investigate the possible advantages of combining techniques of CTGs with CAFs for complicated recession cases. 4. To assess the impact of those interventions on patient-reported outcomes consisting of aesthetics, comfort, and overall satisfaction.
SUBJECTS AND METHODS
This study aims to evaluate the efficacy of different surgical techniques for treating RT2 gingival recessions (Figure 1) through a randomized controlled trial (RCT). Thirty participants with RT2 gingival recessions have been randomly allocated to three groups to evaluate outcomes. Participants had been selected primarily based on inclusion criteria focused on periodontal health and oral hygiene. Those with situations affecting outcomes or prior surgery in the same site were excluded. Randomization was stratified to make certain balanced distributions among groups and locations. Ten subjects each were randomized to connective tissue graft (CTG), coronally advanced flap (CAF), or a combination technique using both strategies. Group assignments aimed to help precisely compare interventions head-to-head with controls. Standardized preoperative assessment and postoperative care protocols had been administered to reduce variability: CTG alone involved creating a partial-thickness flap and securing an autograft harvested from the palate. This aimed to reinforce tissue for coverage without complete root coverage.
In CAF alone, a horizontal incision was made at the gingival margin with two vertical incisions past the mucogingival junction. The flap becomes coronally positioned and sutured over defects to reposition tissue. Careful raising and securing enhance outcomes, however, is based on adequate keratinized width. For the combined approach, a CTG was positioned after flap elevation and secured. The coronally advanced flap was then coronally repositioned and sutured over the augmented area. This capitalized on regenerative and positional benefit to maximize complex case outcomes. Primary and secondary outcomes were evaluated at preferred intervals. As the primary outcomes, percentage of root coverage at six months post-surgery was measured to examine efficacy. Secondary outcomes like clinical attachment levels, keratinized tissue gain, patient-reporting on aesthetics, discomfort, and satisfaction offer a complete assessment of outcomes.
This RCT study design, with nicely defined inclusion/exclusion standards, randomization scheme, and standardized approaches, provided controls essential to carefully examine three groups' approaches for managing RT2 gingival recessions. Evaluating a couple of consequences longitudinally provides more desirable knowledge of the treatment's efficacy over the years.
Figure 1. RT2 gingival recessions related to lower right and left central incisors
Data Collection and Analysis
Data Collection
Two impartial examiners who were blinded to the group assignments completed all measurements. Calibration has been completed to assure inter-examiner reliability.
Statistical Analysis
- Descriptive statistics for demographic and clinical characteristics.
- Paired t-test to compare pre-and post-treatment results within groups.
- ANOVA to compare results among groups.
- A p-value < 0.05 is considered statistically significant.
RESULTS
Participant Demographics and Baseline Characteristics
A total of 30 patients with RT2 gingival recession were enrolled in this study. The participants were randomly assigned to three treatment groups:
1) Group A: Connective Tissue Graft (CTG) alone,
2) Group B: Coronally Advanced Flap (CAF) alone, and
3) Group C: A combination of CTG and CAF.
Baseline demographic and clinical characteristics are shown in Table 1.
Table 1. Baseline Demographic and Clinical Characteristics
|
Characteristic |
Group A (CTG) |
Group B (CAF) |
Group C (CTG + CAF) |
Total |
|
Number of patients |
10 |
10 |
10 |
30 |
|
Age (mean ± SD) |
45 ± 12 |
43 ± 11 |
46 ± 10 |
44.7 ± 11.0
|
|
Gender (M/F) |
5/5 |
6/4 |
4/6 |
15/15 |
|
Maxillary Incisors |
5 |
5 |
5 |
15 |
|
Mandibular Incisors |
5 |
5 |
5 |
15 |
|
Recession Depth (mm) |
3.2 ± 0.5 |
3.0 ± 0.6 |
3.1 ± 0.4 |
3.1 ± 0.5 |
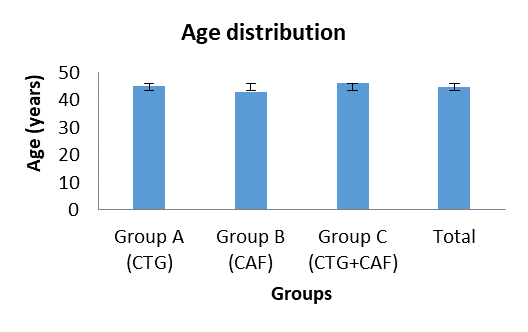
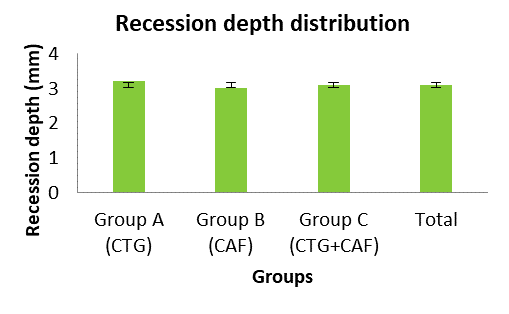
Figure 2 provide insights into participants traits throughout the 3 treatment groups in this clinical trial. Regarding age distribution, the groups have proven similarities based on mean and standard deviation statistics. Specifically, Groups A, B and C had mean ages of approximately 45, 43 and 46 years respectively, indicating age became balanced among groups. Standard deviations were additionally similar between groups, suggesting ages were similarly spread within every sample. Figure 3 shows recession depth distribution, whilst the approach differed barely between groups—with Group A at 3.2 mm, Group B at 3.0 mm, and Group C at 3.1 mm on average—the same Standard deviations have been relatively small. This implies that recession severities tended to be steady inside each group.
Figure 2. Mean age distribution among groups.
Figure 3. Mean recession depth among groups.
Primary Outcome: Root Coverage
The primary outcome of the study was the percentage of root coverage achieved at six months post-surgery. As shown in Table 2, Group C (CTG+CAF) showed the highest mean of root coverage at 82.5%, followed by Group A (CTG) at 75.3% and Group B (CAF) at 68.7%. The differences between the groups was statistically significant (p = 0.03).
Table 2. Root Coverage at 6 Months Post-Surgery
|
Group |
Root Coverage (%) |
Standard Deviation |
p value |
|
Group A (CTG) |
75.3 |
10.2 |
|
|
Group B (CAF) |
68.7 |
12.4 |
|
|
Group C (CTG + CAF) |
82.5 |
8.7 |
0.03* |
*Statistically significant (p < 0.05)
The outcomes provide proof that augmenting CAFs with CTGs is clinically more beneficial compared to single modalities for addressing RT2 recessions. By combining the regenerative capacities and coronal repositioning capability simultaneously, the dual technique appeared best at attaining and keeping root coverage six months post-surgically. This aligns with the speculation that combining strategies ought to maximize profit in complicated cases.
Secondary Outcomes
Clinical Attachment Level (CAL) Gain
The gain in clinical attachment level (CAL) was another critical outcome measured at 6 months post-surgical. As revealed in Table 3, Group C (CTG + CAF) showed the highest CAL gain (2.8 mm), followed by Group A (CTG only) showed 2.4 mm gain and Group B (CAF only) showed 2.1 mm gain. The differences among groups were statistically significant (p = 0.04), indicating better results with the combined technique (Table 3).
Table 3. Clinical Attachment Level Gain at 6 Months Post-Surgery
|
Group |
CAL Gain (mm) |
Standard Deviation |
p value |
|
Group A (CTG) |
2.4 |
0.6 |
|
|
Group B (CAF) |
2.1 |
0.7 |
|
|
Group C (CTG + CAF) |
2.8 |
0.5 |
0.04* |
*Statistically significant (p < 0.05)
Keratinized Tissue Width (KTW) Increase
The increase in keratinized tissue width (KTW) was also assessed at 6 months. Group C demonstrated the highest increase in KTW (1.8 mm), followed by Group A (1.5 mm) and Group B (1.2 mm). These differences were statistically significant (p=0.02), suggesting that the combined approach enhances the width of keratinized tissue more effectively (Table 4).
Table 4. Keratinized Tissue Width Increase at 6 Months Post-Surgery
|
Group |
KTW Increase (mm) |
Standard Deviation |
p -value |
|
Group A (CTG) |
1.5 |
0.5 |
|
|
Group B (CAF) |
1.2 |
0.4 |
|
|
Group C (CTG + CAF) |
1.8 |
0.3 |
0.02* |
*Statistically significant (p < 0.05)
Patient-Reported Outcomes
Patient-reported outcomes provide meaningful insight concerning great life impacts. This study assessed aesthetic satisfaction and discomfort at six months post-operative using a validated visual analog scale (VAS). According to Table 5, Group C reported the highest aesthetic satisfaction (8.6), followed by Group A (8.2) and Group B (7.8). This modest result indicates that patients perceived relatively higher aesthetics from the dual technique on average. Discomfort levels were also compared. While Group C had the lowest reported VAS was3.2 on average, compared to 3.5 and 3.8 in Groups A and B respectively. Although the differences in aesthetic satisfaction approached statistical significance (p = 0.05), they were not significant for discomfort levels (p = 0.06). This implies that while all three techniques gave very similar post-operative comfort in healing and performance over time, participant-focused outcomes point positively to the combination surgical regimen. Six months later, participants were quite pleased aesthetically with the combined technique, despite the fact that there was no significant difference in long-term pain or discomfort. Furthermore, the data support the apparent clinical findings, demonstrating benefits not just for anatomical restoration but also for reported quality of life.
Table 5. Patient-Reported Outcomes at 6 Months Post-Surgery
|
Outcome Measure |
Group A (CTG) |
|
Group B (CAF) |
|
Group C (CTG + CAF) |
p value |
|
Aesthetic Satisfaction (VAS) |
8.2 |
|
7.8 |
|
8.6 |
0.05 |
|
Discomfort (VAS) |
3.5 |
|
3.8 |
|
3.2 |
0.06 |
DISCUSSION
The present study aimed to evaluate and compare the efficacy of different surgical techniques for treating RT2 gingival recessions. The results showed that the combination of CTG and CAF yields superior clinical outcomes as compared to either approach alone. Specifically, the combination approach carried out more root coverage, CAL gain, and KTW increase, along with improved patient reported aesthetic satisfaction. These outcomes are in line with the cutting-edge literature and underscore the significance of using a comprehensive technique to address complicated gingival recession cases.
The main outcome of root coverage in this study showed that the combination method (CTG+CAF) had a mean root coverage of 82.5%, considerably higher than CTG alone (75.3%) and CAF alone (68.7%). These results agree with those reported by Fernández-Jiménez et al. (2021) in their ''systematic review and meta-analysis'', which highlighted that combined surgical approach generally tend to offer higher root coverage results in RT2 gingival recessions [5]. Similarly, Elena et al. (2024) in their randomized clinical trial as well observed that combining a "xenogeneic collagen matrix" with CAF yielded improved root coverage in comparison to the usage of either approach alone [9]. The present study also revealed a considerable CAL gain across all groups, with the combined approach displaying the maximum improvement (2.8 mm). This is consistent with the findings of Rothen et al. (2022), who suggested considerable CAL improvements whilst using subepithelial connective tissue grafts in combination with CAF for treating RT2 recessions. The improved CAL gain achieved with the combination approach can be attributed to the synergistic effect of the graft offering structural support and the flap facilitating the most efficient positioning and healing [10].
Regarding KTW it became markedly higher in the combined group (1.8 mm) in comparison to the other groups. This agrees with the findings of González-Febles et al. (2023), who proved that the tunneled CAF method with connective tissue grafts considerably enhances the width of keratinized tissue [11]. The adequate KTW is essential for long-term periodontal health, as it presents a strong and resilient gingival margin less vulnerable to recession [12]. Patient-reported outcomes indicated the very best aesthetic satisfaction with the combined technique. This finding is supported by Fernández-Jiménez et al. (2024), who noted that patients treated with combined surgical techniques stated higher satisfaction as a result of better aesthetic outcomes and reduced postoperative pain. The significance of aesthetic satisfaction can't be overstated, as it directly impacts patient compliance and overall treatment success [13].
Therefore, the superior results revealed with the combined CTG and CAF approach propose that this technique should be considered the gold standard for treating RT2 gingival recessions. The more desirable root coverage, CAL gain, and KTW increase offer both functional and aesthetic benefits, which are critical for patient satisfaction and long-term periodontal stability.
To attain the best clinical results, clinicians must understand how to use combined techniques to enhance therapeutic outcomes. The findings of this study support the creation of standardized clinical procedures that include a combination of surgical approaches for treating complex gingival recessions. This would ensure uniformity in clinical practice and improve patient outcomes. As Obiechina (2020) highlights, consistent protocols serve to reduce variability in treatment outcomes and improve the predictability of surgical operations [2].
The high levels of patient satisfaction found in this study emphasize the significance of patient education and informed consent. Patients should be aware of the benefits and risks associated with different surgical techniques. Providing thorough information assists patient to make educated decisions and establishes realistic expectations, which is crucial for achieving high satisfaction rates [14,15].
While this study has some useful insights, it is not without limitations. The sample size of 30 patients, while appropriate for a preliminary study, may be insufficient to generalize the findings to a larger population. Furthermore, the six-month follow-up period, while predictive of short-term outcomes, provides little information on the long-term stability of the surgical findings therefore, longer follow-up periods will be scheduled for those patient. Future research with bigger sample sizes and longer follow-up periods are required to validate these findings and examine the treatment outcomes long-term stability.
CONCLUSION
The findings of the current study highlight the superiority of the integration of CTG with CAF in treating RT2 gingival recessions. This combined technique yields higher clinical outcomes in terms of root coverage, CAL gain, and KTW increase, in conjunction with better patient satisfaction. These results are aligned with the cutting-edge literature and assist the adoption of combined surgical approaches for dealing with complex gingival recessions.
Clinicians should remember to include these integrated methods into their practice in order to improve treatment outcomes and patient satisfaction. Furthermore, the development of standardized treatment protocols based only on these data could improve uniformity and predictability in clinical practice. Future studies should focus on long-term outcomes, alternative substances, minimally invasive techniques, and patient-centered techniques in order to further expand the field of recession coverage.
ACKNOWLEDGEMENTS
The authors would like to thank all the participants who took part in this study.
CONFLICT OF INTERESTS
The authors declare no conflict of interest.
FUNDING
The authors received no funding from any organization for the submitted work.
ETHICS APPROVAL
This study followed the principles of the Helsinki Declaration. The Faculty of Dentistry/University of Benghazi's Research Ethics Committee approved the application.
CONSENT TO PARTICIPATE
Informed consent was obtained from all individual participants included in the study.
REFERENCES
- Cairo F, Nieri M, Cincinelli S, Mervelt J, Pagliaro U. (2011). The interproximal clinical attachment level to classify gingival recessions and predict root coverage outcomes: an explorative and reliability study. J Clin Periodontol. 38(7):661-666.
- Obiechina N. (2020). Treating Advanced Gingival Recession: A Review of Treatment Options for Advanced Recession Defects. EC Dental Science. 19(5):54-60.
- Jati AS, Furquim LZ, Consolaro A. (2016). Gingival recession: its causes and types, and the importance of orthodontic treatment. Dental Press J Orthod. 21(3):18-29.
- Cortellini P, Bissada NF. (2018). Mucogingival conditions in the natural dentition: Narrative review, case definitions, and diagnostic considerations. J Periodontol. 89(Suppl 1):S204-S213.
- Fernández-Jiménez A, García-De-La-Fuente AM, Estefanía-Fresco R, Marichalar-Mendia X, Aguirre-Urizar JM, Aguirre-Zorzano LA. (2021). Complete root coverage in the treatment of Miller class III or RT2 gingival recessions: a systematic review and meta-analysis. BMC Oral Health. 21(1):145.
- Ashurko I, Tarasenko S, Magdalyanova M, Bokareva S, Balyasin M, Galyas A, et al. (2023). Comparative analysis of xenogeneic collagen matrix and autogenous subepithelial connective tissue graft to increase soft tissue volume around dental implants: a systematic review and meta-analysis. BMC Oral Health. 23(1):741.
- Lahham C, Ta'a MA. (2022). Clinical comparison between different surgical techniques used to manage advanced gingival recession (Miller's class III & IV). Heliyon. 8(8):e10132.
- Toledano-Osorio M, Muñoz-Soto E, Toledano M, Vallecillo-Rivas M, Vallecillo C, Ramos-García P, et al. (2022). Treating Gingival Recessions Using Coronally Advanced Flap or Tunnel Techniques with Autografts or Polymeric Substitutes: A Systematic Review and Meta-Analysis. Polymers (Basel). 14(7):1453.
- Elena RD, Miren VF, Ana-María GD, Xabier MM, Luis-Antonio AZ. (2024). Analysis of the treatment of RT2 recessions with a xenogeneic collagen matrix vs. connective tissue graft combined with a coronally advanced flap. A double-blinded randomized clinical trial. Clin Oral Investig. 28(4):215.
- Rothen SK, Silva EO, Bin LR, Nassar PO, Nassar CA. (2022). Clinical Comparison of Two Surgical Techniques in the Treatment of Cairo RT2 Gingival Recessions Associated to Subepithelial Connective Tissue Graft: Randomized Clinical Trial. J Adv Med Med Res. 34(23):171-181.
- González-Febles J, Romandini M, Laciar-Oudshoorn F, Noguerol F, Marruganti C, Bujaldón-Daza A, et al. (2023). Tunnel vs. coronally advanced flap in combination with a connective tissue graft for the treatment of multiple gingival recessions: a multi-center randomized clinical trial. Clin Oral Investig. 27(7):3627-3638.
- Kumar S, Hirani T, Shah S, Mehta R, Bhakkand SR, Shishoo D. (2020). Treating Public Health Dilemma of Gingival Recession by the Dehydrated Amnion Allograft: A 5-Year Longitudinal Study. Front Oral Health. 1:540211.
- Fernández-Jiménez A, García-De-La-Fuente AM, Marichalar-Mendia X, Aguirre-Zorzano LA, Estefanía-Fresco R. (2024). Treatment of deep single RT2 and RT3 antero-mandibular gingival recessions with a combination of surgical techniques: A case series study. J Esthet Restor Dent. 36(2):363-372.
- Stefanini M, Jepsen K, de Sanctis M, Baldini N, Greven B, Heinz B, et al. (2016). Patient-reported outcomes and aesthetic evaluation of root coverage procedures: a 12-month follow-up of a randomized controlled clinical trial. J Clin Periodontol. 43(12):1132-1141.
- Yeragi ES, Nalawade KP, Gotmare SA, Benjamin A, Putta V, Lavekar A. (2021). Surgical management of RT2 gingival recession using sub epithelial connective tissue graft and coronally advanced flap: A case report. J Dent Panacea. 3(3):138-142.
 Abstract
Abstract  PDF
PDF